Investigators:
Rebecca Spencer, UMass Amherst
MassAITC Cohort: Year 2 (AD/ADRD)
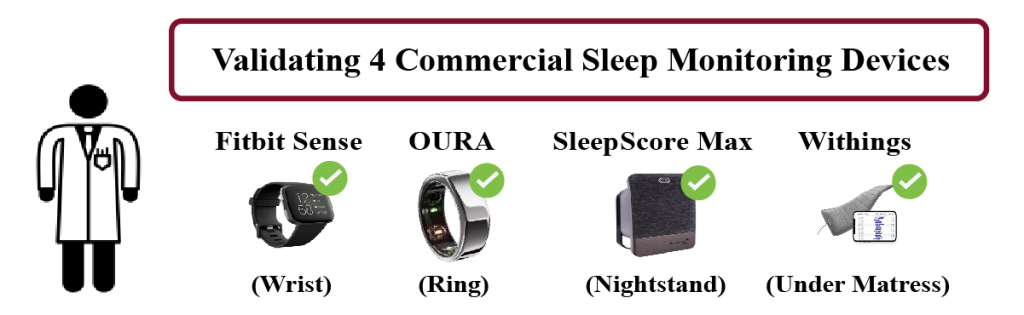
Project Accomplishments: The pilot project aimed to validate the accuracy and usability of commercial sleep tracking devices in older adults, including those with Alzheimer’s disease (AD), related dementias (ADRD), or mild cognitive impairment (MCI). Participants aged 60–90 used four devices—Fitbit Sense 2, Withings bed mat, Oura ring, and Sleep Score Max—over seven nights, with polysomnography (PSG) used as the gold standard for comparison. While recruitment of participants with AD/MCI proved challenging, the study successfully collected comprehensive data from 20 cognitively healthy older adults and a smaller number of MCI participants. Results showed that all devices significantly underestimated total sleep time compared to PSG, with the Withings bed mat performing best in terms of usability and data completeness, especially among participants with cognitive impairment.
The study also included a longitudinal component, where participants used selected devices for up to 28 days. High compliance and usability were observed, particularly with the Withings bed mat, which required minimal user interaction. Subjective usability ratings further supported this finding, with the Withings device scoring highest among both cognitively normal and MCI participants. The project’s key outcome is a publicly accessible dataset being uploaded to the National Sleep Research Resource, which includes PSG and device data. These findings highlight the need for caution when using commercial sleep trackers in older adults and underscore the importance of validating such tools in populations with cognitive decline.
Initial Proposal Abstract: Easily accessible, user friendly, and validated in-home sleep monitoring technologies are in high research, commercial, and clinical demand for older adults. Monitoring multiple physiological signals in patients’ homes provides a promising opportunity for clinicians to improve treatment outcomes and conveniently access relevant health metrics in older adults. Novel commercial and research grade devices are constantly evolving to meet growing demand from consumers and increase accuracy. To improve accuracy, more and more devices are integrating a wider array of physiological processes (e.g., heart rate, SpO2, ECG). However, scientific validation studies examining the accuracy and performance of these devices is minimal and completely absent in older adults with common chronic conditions and in individuals with Alzheimer’s disease and Alzheimer’s related dementias (AD/ADRD). Yet targeted studies in these groups are necessary given aging- and AD-related changes in gait, mobility, and physiological processes that may decrease the accuracy of devices.
This study seeks to validate sleep detection capabilities of commercially available devices with physiological sensors in a diverse representative sample of older adults with common chronic conditions and a group with AD/ADRD. Device performance will be examined in in-home settings and compared to gold-standard sleep measures (polysomnography – a montage of EEG, EMG, and EOG). Further, with a series of questionnaires, we will identify high-utility device features, barriers to use, and other aspects relevant to improving future device development and compliance in both research and commercial settings. We consider this an essential first step towards deploying devices for health and research.
Outcomes:
- Publication: Validation of commercial sleep-tracking wearables and nearables in healthy young and older adults
 Authors: M.E. Searles, A. Licata, M. Cucinotta, K. Kainec, and R.M.C. Spencer Abstract Study objectives: Changes in sleep with aging are associated with risk for Alzheimer’s and other neurological diseases, risk of accidents, and can be a predictor of health decline. For this reason, continuous sleep monitoring is of great… Read more: Publication: Validation of commercial sleep-tracking wearables and nearables in healthy young and older adults
Authors: M.E. Searles, A. Licata, M. Cucinotta, K. Kainec, and R.M.C. Spencer Abstract Study objectives: Changes in sleep with aging are associated with risk for Alzheimer’s and other neurological diseases, risk of accidents, and can be a predictor of health decline. For this reason, continuous sleep monitoring is of great… Read more: Publication: Validation of commercial sleep-tracking wearables and nearables in healthy young and older adults - Poster Presentation: a2 National Symposium 2024
 Title: Validating Novel Sleep Sensors and Devices in Older Adults Authors: Matthew Cucinotta, Kyle Kainec, Mary Emma Searles, Rebecca Spencer
Title: Validating Novel Sleep Sensors and Devices in Older Adults Authors: Matthew Cucinotta, Kyle Kainec, Mary Emma Searles, Rebecca Spencer
